A University of Virginia Health System program that provides follow-up care for heart failure patients after they leave the hospital significantly improves survival and other outcomes while saving money, a new study finds.
The study examined participants between January 2011 and December 2014 in UVA’s Hospital-to-Home (H2H) program, which is available to all heart failure patients that live within 90 miles of UVA Medical Center. For 30 days after they are released from the hospital, patients can have follow-up visits and other support from two nurse practitioners specializing in heart failure.
In the first 30 days after being released from UVA, program participants had a 41 percent lower mortality rate and a 24 percent reduction in the number of days they were re-admitted to the hospital compared with patients that did not participate in the H2H program during this timeframe. These improvements in outcomes occurred even though H2H participants were sicker than non-participants, the study found.
The cost savings from the program were estimated to be about twice as much as the program’s staffing costs. This is especially valuable because other studies have shown that heart failure care – which cost an estimated $31.7 billion in 2012 and is projected to more than double by 2030 – is a leading driver of healthcare costs in the U.S.
Keys to Success
Because heart failure is a chronic disease, ongoing management of each patient’s care is key to good outcomes, said Sula Mazimba, MD, MPH, a study co-author and a heart failure specialist at UVA.
“It’s important to have a program that follows patients closely and especially during their most vulnerable period following a discharge from the hospital. In this regard, a discharge from the hospital is not really a final goodbye, but rather just another phase of their care,” he said.
Within a week of being released from the hospital, patients typically have an in-person visit with one of the program’s nurse practitioners. Working with UVA physicians, pharmacists and other team members, the nurse practitioners assess patients’ heart failure symptoms and lab results, adjust their medications as needed and suggest lifestyle adjustments such as dietary changes.
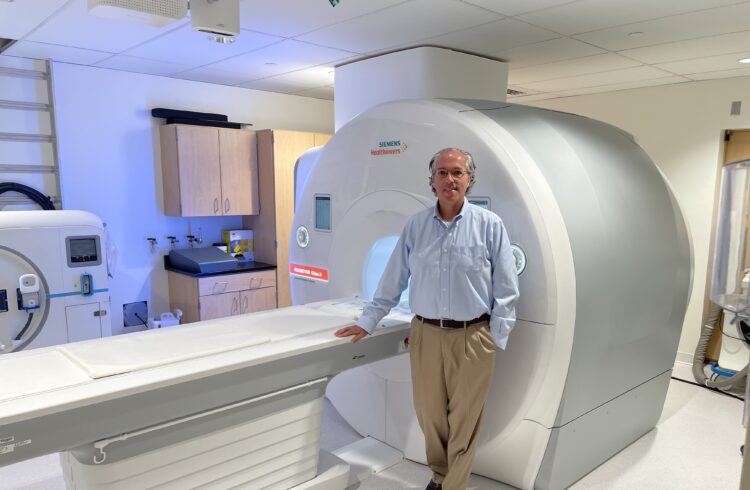
“It’s a collaborative, multidisciplinary approach,” said study co-author Kenneth Bilchick, MD, MS, a member of UVA’s heart and vascular team. “We take a holistic view of what needs to be done to keep patients out of the hospital.”
Findings Published
Bilchick, Mazimba and their colleagues have published their findings in the American Journal of Medical Quality. Their research team consisted of Travis Moss, Timothy Welch, Wayne Levy (University of Washington), George Stukenborg, Bryan T. Lawlor, Juanita Reigle, S. Craig Thomas, Carolyn Brady, James D. Bergin, Jamie L.W. Kennedy, Mohammed Abuannadi and Kenneth Scully.