Nearly one million Americans today require 24/7 supplemental oxygen therapy to help them breathe. Ruth McCoy, a former respiratory therapist from New Market, Virginia, is one of them.
McCoy, who suffers from advanced lung disease, began relying on supplemental oxygen in January 2007. While her small oxygen tank could be conveniently carried like a purse, McCoy often experienced discomfort while wearing the facial apparatus that went with it. Called a nasal cannula, it consisted of plastic tubing that tucked behind her ears and connected to prongs inside her nostrils. She had other concerns. “People stared at me when I was in public. It would come loose when I was sleeping and got in the way when I was eating or went to kiss my husband,” she says.
While working as a respiratory therapist, McCoy had heard that an alternative to the cannula had been developed and received FDA approval. Her pulmonologist agreed that she would be a good candidate for the device – a catheter that delivered oxygen through her trachea – and began searching for a provider. “I was surprised to learn that these devices are not as widely available as I thought,” McCoy says.
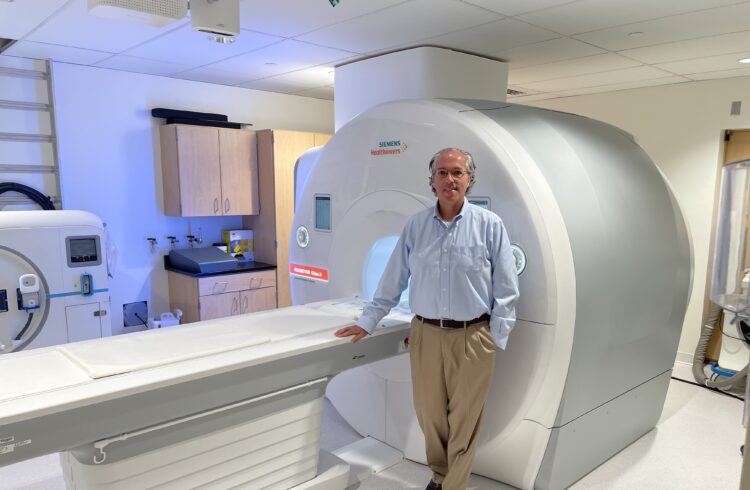
Ultimately, McCoy connected with Dr. Christine Lau, a cardiothoracic surgeon at the University of Virginia Health System. Last month, Dr. Lau placed McCoy under local sedation, made a small incision and inserted a stent into her trachea. McCoy spent the night at UVA Medical Center and was discharged the next day, after Dr. Lau inserted the catheter through the stent.
During her first weeks on the new therapy, McCoy visited Dr. Lau twice a week to ensure that she adapted well. “The new system is great,” reports McCoy. “I’ve been able to cut my oxygen flow by half. Plus, I have more energy than before because the oxygen is going directly into my lungs.”
McCoy now sets her oxygen flow at 1 liter while resting, 1.5 liters while sleeping and 3 liters when she is active. When wearing the cannula, her flow rates were 3 liters while resting, 3.5 liters when sleeping and 4.5 liters during activity.
Another big benefit, says McCoy, is that she wears the catheter on a necklace that can be changed and coordinated with her outfit and, if she wants, hidden by a scarf. Her oxygen tubes are now out of sight, worn under her clothes.
Dr. Lau is encouraged by McCoy’s success and believes this innovative therapy could increase the quality of life for other patients using supplemental oxygen. Those most likely to benefit by switching to the transtraceal system include patients with end-stage lung disease such as emphysema, COPD, and pulmonary fibrosis .