Timothy Showalter, MD, has determined that offering the best treatment for cervical cancer actually costs hospitals money. This can leave the hospitals -- and their patients -- in the lurch.
The evidence is clear: Cervical cancer is best treated with brachytherapy, a form of radiation therapy. Yet the use of this potentially lifesaving treatment has been declining, and a new study from the School of Medicine may explain why.
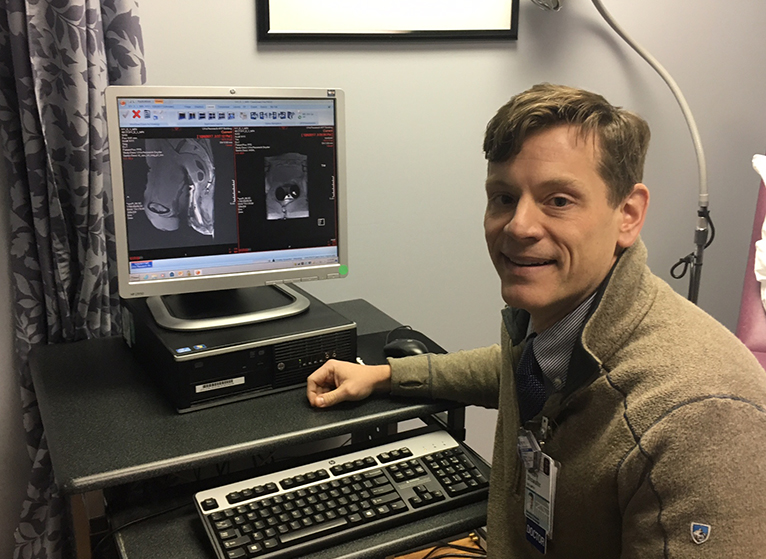
UVA researchers have determined that offering brachytherapy for locally advanced cervical cancer actually ends up costing hospitals money. After accounting for the costs and time involved, the researchers found that Medicare reimburses four times more per minute required for a less effective alternative than it does for brachytherapy. Ultimately, providing brachytherapy results in a net loss for the providing healthcare facility, the researchers determined. This can leave hospitals – particularly smaller hospitals that don’t do a lot of brachytherapy – in the lurch.
“Studies have time and time again shown that brachytherapy is the most important part of cervical cancer treatment, because it is essential to eradicating the tumor,” said Timothy Showalter, MD, a radiation oncologist at UVA Cancer Center. “A decline in brachytherapy utilization is associated with a higher rate of mortality in cervical cancer, so there’s a direct relationship.”
Treating Cervical Cancer
The problem stems partly from the amount of physician time brachytherapy requires: It takes 80+ percent more personnel time to administer brachytherapy than it does to deliver the increasingly popular alternative, external beam radiation. Both methods deliver radiation to the tumor, but brachytherapy delivers much greater doses in a much more targeted manner. Another key difference, the researchers found: Medicare reimbursement makes external beam radiation profitable, while brachytherapy is not.
Overall, the researchers determined that it costs hospitals more than twice as much to provide brachytherapy as it does to provide external-beam radiation. But the reimbursement doesn’t reflect that.
“Brachytherapy requires a lot of physician effort and expertise and reimburses poorly for that effort,” Showalter said. “I can certainly imagine how the comparatively poor reimbursement rates compared to external beam radiation could contribute in some environments to not establishing a service for brachytherapy or just not committing physician time to it.”
He noted that healthcare providers face a cold, hard truth when deciding whether to offer brachytherapy, or any other treatment: “If practices don’t run at least a profit greater than zero,” he said, “then they fold.”
Best Places for Brachytherapy
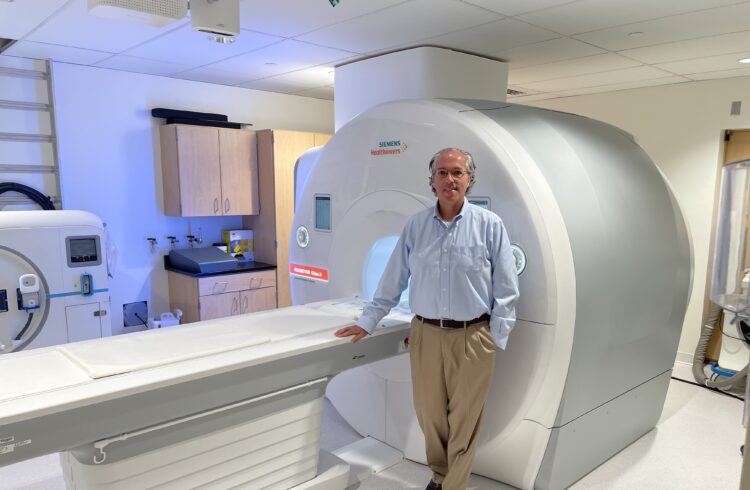
The researchers concluded that hospitals that see a high volume of patients, such as UVA, are best equipped to provide brachytherapy – and to absorb the major resource commitment that comes with it. “My job specifically involves brachytherapy,” Showalter said. “We’re at this big hospital with all the equipment we need at the ready and a wonderful streamlined process that enhances the patient experience and reduces patients’ time on the table. That makes it easier to provide efficient and effective care.”
“At UVA, we are particularly proud of our brachytherapy program and delivering quality brachytherapy is a top priority for us,” he said. “We are fortunate that these financial considerations have not impacted our center, but these pressures could be a real barrier for smaller centers.”
He expressed grave concern about the declining use of brachytherapy: “It’s disturbing because we have this great treatment option that’s an absolute requirement of curative therapy, and it’s been available for decades, but the rates of actually using it are dropping,” Showalter said. “It’s like if you had an effective drug and people stopped using it.”
Findings Published
The researchers have published their findings in the International Journal of Radiation Oncology. The paper was authored by Kristine Bauer-Nilsen, Colin Hill, Daniel M. Trifiletti, Bruce Libby, Donna H. Lash, Melody Lain, Deborah Christodoulou, Constance Hodge and Showalter.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.
RELATED: Showalter aims to help men with prostate cancer make complex care decisions.