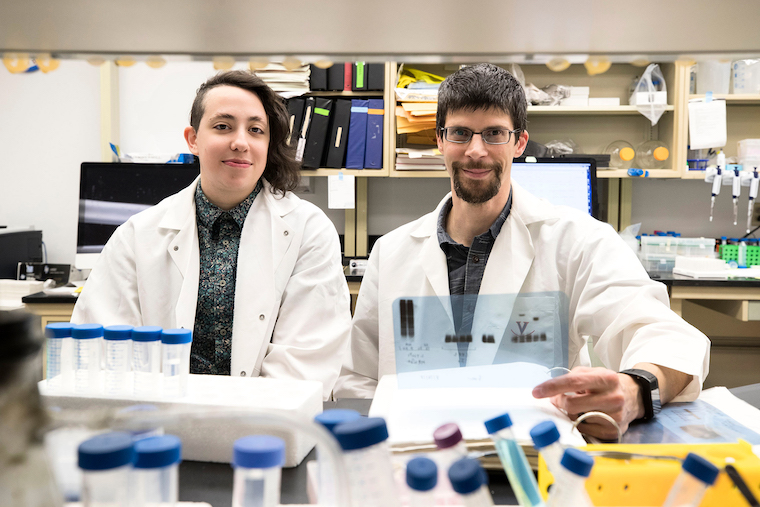
Dorian A Rosen, PhD, (left) and Alban Gaultier, PhD, found last year that fluvoxamine may stop the deadly inflammation known as sepsis. The drug is now being tested as a protective measure for patients with COVID-19.
The antidepressant fluvoxamine appears to prevent COVID-19 infections from worsening and may help keep patients out of the hospital, a trial based on research from the School of Medicine suggests.
The clinical trial, conducted by the Washington University School of Medicine in St. Louis, compared fluvoxamine with a placebo in 152 adult outpatients infected with the coronavirus. None of the 80 participants who received fluvoxamine became seriously ill after 15 days, while six patients who received placebo did. Of those six, four were hospitalized, for periods ranging from four to 21 days. One was on a ventilator for 10 days.
While the study size was small, the researchers say the results are statistically significant and that fluvoxamine warrants further study as a COVID-19 treatment. They plan to launch a larger trial in the next few weeks.
“The patients who took fluvoxamine did not develop serious breathing difficulties or require hospitalization for problems with lung function,” said Eric J. Lenze, MD, of the Washington University School of Medicine. “Most investigational treatments for COVID-19 have been aimed at the very sickest patients, but it’s also important to find therapies that prevent patients from getting sick enough to require supplemental oxygen or to have to go to the hospital. Our study suggests fluvoxamine may help fill that niche.”
Fluvoxamine and COVID-19
The Washington University researchers launched the randomized, double-blind trial based on a discovery by UVA’s Alban Gaultier, PhD, and former graduate student Dorian A Rosen, PhD. Gaultier and Rosen found last year that fluvoxamine may stop the deadly inflammation known as sepsis, in which the immune response spirals out of control. The drug, they determined, reduced the production of cytokines, which have been linked to potentially deadly “cytokine storms” thought to occur in severe cases of COVID-19.
That connection prompted the Washington University team to investigate the possibility that fluvoxamine could have a protective effect for patients with COVID-19. Perhaps, they thought, the drug could help prevent the immune system overreactions triggered by this strange new coronavirus. And their work suggests it may.
“Because elevated cytokines levels have been associated with COVID-19 severity, testing fluvoxamine in a clinical trial made a lot of sense to us,” said Gaultier, of UVA’s Department of Neuroscience and its Center for Brain Immunology and Glia (BIG). “We are still unclear about the mode of action of fluvoxamine against SARS-CoV-2, but research is under way to find the answer.”
The Washington University team noted that recent research has raised questions about whether cytokines are really playing important roles in COVID-19 deaths. If not, the researchers say, fluvoxamine may be having beneficial effects by some other mechanism not yet understood.
“There are several ways this drug might work to help COVID-19 patients, but we think it most likely may be interacting with the sigma-1 receptor to reduce the production of inflammatory molecules,” said Washington University’s Angela M Reiersen, MD. “Past research has demonstrated that fluvoxamine can reduce inflammation in animal models of sepsis, and it may be doing something similar in our patients.”
The researchers stressed that there were several limitations to their research. In addition to its small size, the trial was hampered by other factors, including that 20% of participants stopped answering surveys during the 15-day trial. (The researchers determined that none of those participants required hospitalization or emergency-department visits, but they could not rule out that the participants sought treatment elsewhere, such as at urgent-care clinics.)
Because of these limitations, the researchers say that the trial’s results should not be treated as a measure of fluvoxamine’s effectiveness against COVID-19 but as an encouraging indicator that the drug warrants further testing.
“If a larger clinical trial (phase III) confirms the results, fluvoxamine would be a perfect treatment for COVID patients newly diagnosed,” Gaultier said. “Fluvoxamine is not an experimental drug, it is cheap and safe and could be available as a first line of defense to unburden the hospitals that are overwhelmed by the COVID health crisis.”
Findings Published
The researchers have published their findings in the Journal of the American Medical Association. The Washington University team consisted of Lenze, Caline Mattar, Charles F. Zorumski, Angela Stevens, Julie Schweiger, Ginger E. Nicol, J. Philip Miller, Lei Yang, Michael Yingling, Michael S. Avidan and Reiersen. A list of the authors’ disclosures is included in the paper.
The clinical trial was supported by the Taylor Family Institute for Innovative Psychiatric Treatment at Washington University and the COVID-19 Early Treatment Fund. Additional support was provided by the Center for Brain Research in Mood Disorders at Washington University, the Bantly Foundation and National Institutes of Health grant UL1TR002345.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.