A sweeping new international report looks at the potential of "precision medicine" to improve diabetes care.
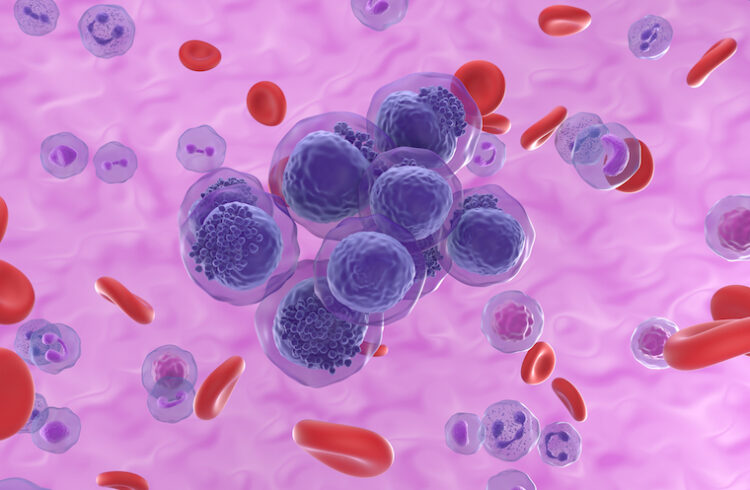
Cutting-edge “precision medicine” has great potential to advance the diagnosis, treatment and ultimate prevention of different forms of diabetes, an international coalition of scientists reports in a sweeping assessment of the state of the field around the world.
The new international “consensus report” was compiled by more than 200 experts from 28 countries, reviewing the published scientific literature. It highlights areas where precision medicine has already transformed diabetes diagnosis, prevention, treatment and monitoring. But it also serves as a roadmap to the future, identifying areas where research is critically needed and recommending steps that can be taken right away to improve patient care.
“The work by this international consortium has taken over three years, all by volunteer effort, determining where precision diabetes medicine works and, more importantly, what are the knowledge gaps and barriers to implementation,” said the University of Virginia School of Medicine’s Stephen S. Rich, PhD, co-chair of the Precision Medicine in Diabetes Initiative (PMDI) that produced the report. “Diabetes is a heterogeneous disease, and the classical definitions of type 2 diabetes, for example, is overly simple and leads to issues of diagnosis (is it really type 2 diabetes?), treatment (what drug is best to achieve normal blood sugars, or is behavioral change, such as increased exercise and/or improved diet, sufficient?), and prognosis (is there increased risk of heart disease, kidney disease or other complication of diabetes that requires more intensive follow-up and monitoring?). Critically, we need to develop an understanding of the heterogeneity of diabetes that can be applied globally, and not to only the well-resourced countries and groups.”
About Diabetes Precision Medicine
Personalized medicine is tailored to the individual, instead of providing the same treatments to everyone, as has been traditionally the case. This approach is mostly known in cancer research, where individual treatments are determined for each person. In contrast, precision medicine is based upon identifying groups of people with similar disease characteristics and similar responses to treatment and risks of complications. Precision diabetes medicine incorporates information about a person’s genes, lifestyle and other factors to ensure each person gets the care that will work best for him or her. The result of precision medicine is to increase the ability of personalized medicine to have the correct effect and improved outcomes, bespoke to each person.
To assess where diabetes precision medicine stands and the potential it holds, the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) convened the Precision Medicine in Diabetes Initiative in 2018. The initiative’s new consensus report – its second – shows important progress in the implementation of the approach. For instance, precision medicine plays an essential role in diagnosing and treating many forms of monogenic diabetes (a type of diabetes caused by a single gene mutation, representing 2%-3% of all forms of diabetes), thanks to major advancements in genetic testing.
“In the field of monogenic diabetes, precision medicine holds a lot of promise because one can achieve a very precise diagnosis using genomics, which guides treatment choices,” said Paul Franks, PhD, chair of the report and scientific director in medical science and head of translational medicine at the Novo Nordisk Foundation.
While all forms of diabetes have a genetic basis, it is only in the monogenic forms of diabetes that a known single mutation can provide a certain diagnosis and optimal treatment plan; other forms of diabetes have many genetic variants and non-genetic factors that contribute to risk.
Near-Term Applications for Precision Medicine
Precision medicine also shows potential in managing gestational diabetes, a form of diabetes that can occur in mothers during pregnancy and increases risk of type 2 diabetes in both the mother and child, the report notes. Specific maternal characteristics have been identified as predictive factors for the success or failure of treatment, including age, body-mass index (BMI) and family history of diabetes.
In the context of type 1 diabetes prevention, the report identifies genetic risk classification as one of the most promising areas for immediate clinical implementation. Recent work by UVA researchers led by Rich has identified 90% of the genetic risk of type 1 diabetes. With this information, doctors can look at children’s genetic risk to determine if they have increased chances of developing type 1 diabetes. For those at highest risk, doctors can screen for the presence of islet autoantibodies that indicate that the immune system is attacking the body’s insulin-producing beta cells; this can allow the introduction of important immune interventions.
For type 2 diabetes, the consensus report presents evidence that routine clinical features can help predict how well different types of drugs work at treating the condition. The report also suggests how this common form of diabetes (almost 90% of all diabetes) can be sub-classified into more precise sub-types.
While the consensus report highlights areas where precision medicine can improve clinical practice, it also draws attention to research gaps and the need for improved research methods.
“A series of gaps in knowledge were identified by the experts that cut across all forms of diabetes,” said Rich,of UVA’s Center for Public Health Genomics and the Department of Public Health Sciences. “It became clear that the published findings were predominantly in people of European Caucasian ancestry, from well-resourced countries, and often did not provide strong statistical support for their results. As a result, more work in diverse populations is needed, to include use of multiple data sources, development of scalable and inexpensive assays for biomarkers, understanding both clinical and social/behavioral factors and consideration of diabetes across the lifespan.”
Findings Released
Franks presented the main findings of the consensus report at the EASD Annual Meeting in Hamburg, Germany, this month. The report was published in Nature Medicine to coincide with the EASD symposium. Simultaneously, the systematic evidence reviews summarized in the consensus report are being published in Communications Medicine, and a parallel series of papers on precision medicine will be published in The Lancet Diabetes & Endocrinology.
The project was supported by the American Diabetes Association, the European Association for the Study of Diabetes and the Novo Nordisk Foundation.
To keep up with the latest medical research news from UVA, subscribe to the Making of Medicine blog.